Shoulder
ROTATOR CUFF TEARS
Tears to your rotator cuff can happen in a variety of ways. They can occur from repetitive trauma, a single injury, or be degenerative in nature. Depending on your symptoms and the severity of the tear, treatment can vary.
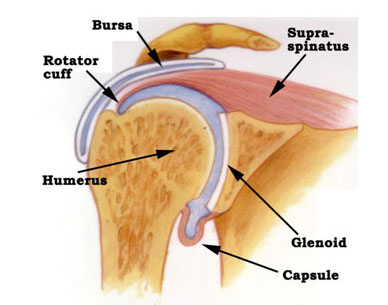
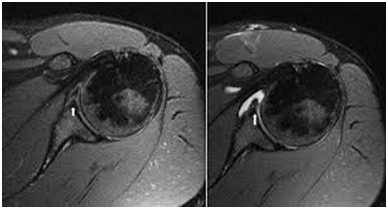
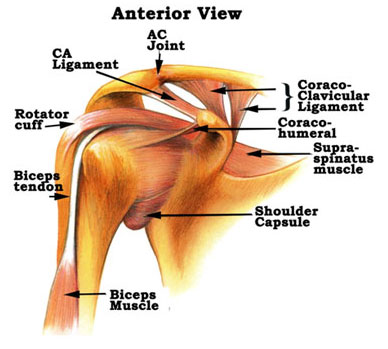
The rotator cuff is made up of the tendons belonging to four muscles inside the shoulder. These muscles are responsible for stability and function of the shoulder joint. Symptoms associated with tearing include pain in the front and outside portion of the shoulder, radiating pain to the upper arm area, weakness in the shoulder, and nighttime pain. Diagnosis is confirmed with a good quality MRI.
Treatment for this type of injury involves both surgical and nonsurgical options. Symptomatic relief can be found with oral anti-inflammatories or a cortisone injection inside the shoulder, ice regimen and physical therapy. Often times, if the rotator cuff tear is small, the above measures are all you need to return to back to activity. However, larger tears or recurrently symptomatic tears may require surgery.
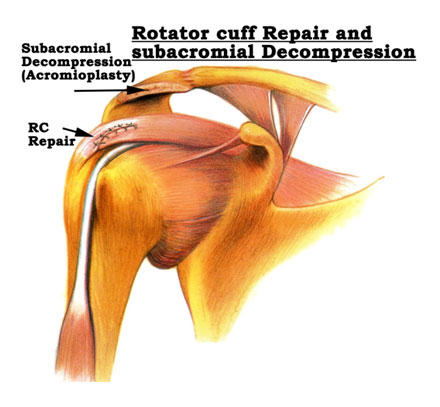
Surgery for this injury is done arthroscopically. Three or four small incisions are made around the shoulder for a minimally invasive approach. The rotator cuff is reattached to its footprint on the humerus with small suture anchors that allow the tendon to heal over time. Along with your rotator cuff repair, an acromioplasty or decompression is done to make more room for your rotator cuff to function. Recovery after surgery involves sling immobilization for approximately four to six weeks followed by physical therapy to regain motion and strength.
Click here to read more about this surgery and the recovery process.
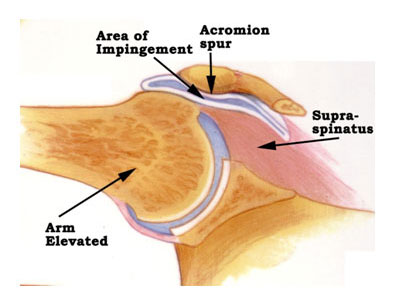
SHOULDER IMPINGEMENT
Like rotator cuff tears, shoulder impingement can occur in a variety of ways. Most often, it is from repetitive trauma. Under your acromion bone, a small bursal sac that overlies your rotator cuff. If you have down-sloping, or a spur, of your acromion the space for your bursa and rotator cuff is diminished. This, along with repetitive trauma, places you at risk for developing impingement. The symptoms of impingement include pain in the front and outside portion of the shoulder when activities are performed at or above shoulder level. An MRI is helpful in establishing the diagnosis and ruling out any rotator cuff tearing.
Treatment for this issue involves reducing bursal inflammation. This can be accomplished with oral anti-inflammatories or a cortisone injection inside the shoulder. Physical therapy is also recommended to reduce inflammation and strengthen the shoulder joint.
Occasionally, impingement symptoms can become chronic and recurring. If that is the case, an arthroscopic decompression of the acromion bone with debridement of the bursa can be performed.
Click here to read more about this surgery and the recovery process.
SHOULDER LABRAL TEARING
Your shoulder is a ball and socket joint, and holding together this joint is a structure called the labrum. The labrum is a series of ligaments that provide stability to the shoulder. Tears in the labrum can occur in a number of ways; traumatic dislocation, repetitive trauma, or a single injury. Pain associated with these tears can include frank instability or sensation of loosening of the joint, vague achiness or discomfort, clicking or catching inside the shoulder. Diagnosis is confirmed with an MRI arthrogram.
Treatment for labral tears involves both surgical and non-surgical options. Depending on symptoms, and the nature of the tear, surgical labral repair with suture anchors may be necessary to fix the labrum back down to the bone. Conservative treatment involves reducing inflammation and strengthening the joint with physical therapy.
Click here to read more about this surgery and the recovery process.
SHOULDER DISLOCATION AND INSTABILITY
Our shoulders have the greatest mobility of all our joints. With this increased mobility comes the cost of instability. Instability of the shoulder can result from traumatic dislocation or slowly progress with continuous trauma. The labrum, or ligaments surrounding the shoulder joint, is responsible for your shoulders’ stability. Tears of these ligaments, or labrum, can cause chronic and recurrent instability.
Traumatic instability, following a dislocation, involves rupture of the labrum of the socket. When dislocation occurs, particularly in young and athletic patients, recurrent dislocations and instability are common. Treatment is initially aimed at reducing inflammation and motion. Should conservative measures fail, and recurrent instability be an issue, surgical reconstruction of the labrum is a good option.
Minimal invasion arthroscopic surgery is utilized to reattach the torn labrum back onto the glenoid bone using small suture anchors. This allows the labrum to heal and re-stabilizes the shoulder. Recovery from this procedure involves sling immobilization for about four weeks followed by good aggressive physical therapy to regain motion and strength.
Patients with non-traumatic instability of the shoulder, either from continuous trauma or naturally loose ligaments, rarely have tearing of the labrum. Treatment in this case involves stabilizing and strengthening the shoulder with physical therapy.
SHOULDER ARTHRITIS
Shoulder osteoarthritis is normal wear and tear on the joint that results in destruction of the cartilage that covers the ball and socket. Eventually, as this cartilage continues the wear out, there in bone on bone contact. Most common symptoms associated with shoulder arthritis are pain and stiffness. Once cartilage is lost, it cannot be replaced. Symptoms can be managed with medication and physical therapy to reduce pain and increase functionality. However, ultimately a shoulder replacement may be needed.
Shoulder replacements can be done in one of two ways. A traditional shoulder replacement and a reverse shoulder replacement. Surgical technique for both procedures is similar. Which surgery option is right for you depends on the integrity of your rotator cuff. Those with intact rotator cuffs can proceed with a traditional replacement. Patients with chronically torn rotator cuffs will require a reverse joint replacement in which the positioning of the ball and socket it reversed. This method takes away the need for a functioning rotator cuff.
Regardless of which surgical procedure you have, recovery involves six weeks of sling immobilization followed by good physical therapy to regain range of motion and strength.
FROZEN SHOULDER
Frozen shoulder, or adhesive capsulitis, is a painful stiffening of the shoulder capsule that results in restricted range of motion. This often occurs without specific cause, although it can be associated with trauma. It is most common in patients 40 to 60 years old and has some affinity for patients with diabetes or thyroid issues. Symptoms associated with frozen shoulder include progressive stiffness and pain. Diagnosis is made via physical exam and although MRI is helpful in ruling out concurrent issues inside the shoulder, it is not usually necessary.
Treatment for this involves aggressive physical therapy to stretch out the capsule and regain motion. A cortisone injection inside the shoulder is also recommended to reducing inflammation, pain, and scar tissue. Often times, physical therapy and an injection alone will resolve the issue. However the need for more aggressive treatment may be needed.
Two surgical procedures are available to resolve more refractory cases. A manipulation under anesthesia is one such procedure. This involves passive range of motion of the affected shoulder while the patient is asleep under anesthesia. This will manually break up the capsule that has gotten tight and scarred. Following this procedure aggressive physical therapy is started to keep the capsule from tightening again.
Should this procedure fail, a second, arthroscopic option is available. This involves making three small incisions around the shoulder and using a camera to look inside the joint and physically open the capsule with arthroscopic scissors. This allows the capsule to open and heal in an elongated position. Physical therapy is again initiated post operatively to keep the capsule from tightening and scaring.