Foot & Ankle
ANKLE SPRAIN AND ANKLE INSTABILITY
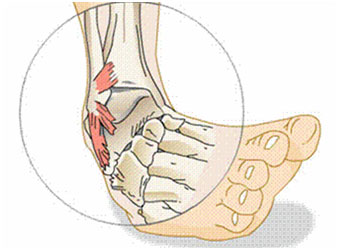
Ankle sprains are a very common injury and can affect all patient populations. Ankle sprains happen when the foot twists or rolls beyond its normal force. This severe in-turning or out-turning of the foot relative to the ankle causes the supporting ligaments to stretch beyond their normal length. In some cases the force is so strong that the ligaments tear. Some patients may even hear a loud “pop”.
Symptoms of ankle sprains include swelling, pain, bruising and often instability of the ankle when walking. Diagnosis is based on history of the injury and physical exam. X-rays are helpful to rule out any fractures, and MRIs can confirm the suspected diagnosis or be helpful if symptoms persist longer than expected.
Initial treatment for an ankle sprain is conservative; rest, ice, elevation, and anti-inflammatories. Oftentimes crutches and a removable walking boot are needed in the early days following the injury to give patients support and stabilization. Once the acute pain and inflammation has resolved, physical therapy is recommended to begin building strength and stability in the ankle while the ligaments continue to heal.
Majority of patients do well with conservative care and have resolution of their symptoms within three to four months. Unfortunately some ankle sprains are still symptomatic six months after injury. Patients in this group often continue to have ankle instability despite conservative care and may require a surgical procedure to tighten the injured ligaments.
Head to our “Treatments” section to read more about this surgery and the recovery process
ACHILLES TENDONITIS/ACHILLES TENDON RUPTURE
Achilles tendonitis is a common condition that causes pain over the back of the ankle and heel. The Achilles tendon is a large tendon that connects your calf muscle to your heel. Your Achilles is needed for walking, running, and jumping.
Tendonitis of the Achilles is inflammation of the tendon that results from repetitive trauma. Patients often complain of tightness in the calf, pain that worsens with activity, swelling over the tendon, and thickening of the tendon. Diagnosis is made via physical exam. X-rays are helpful to evaluate for any bone spurs at the attachment site of the Achilles and sometimes an MRI is needed to rule out any partial tearing of the tendon.
Treatment is generally conservative. Ice, anti-inflammatories, and an aggressive stretching regimen are needed. All impact activities such as running and jumping should be stopped until the Achilles has healed to prevent tendon rupture.
It may take some time for symptoms to resolve as Achilles tendonitis can become chronic. A relatively new option for the treatment of chronic Achilles tendonitis is PRP (platelet rich plasma) injections. Please head to our section on “PRP” to read more about this. Should all conservative care fail surgical debridement can be done to remove chronic scar tissue from the tendon.
Achilles tendon rupture a traumatic injury to the Achilles that causes the tendon to tear. Tears can either be at the attachment site or within the substance of the tendon. This injury usually happens while running or jumping and is most common is men over 40 years old. Treatment for this is surgical.
After an acute Achilles rupture patients will have pain, swelling, bruising, difficulty walking, and palpable deformity to the Achilles. MRI confirms the diagnosis.
Surgery aims at reattaching the Achilles. This can be done by suturing the two ends together or anchoring the tendon back to its bony attachment on the heel, depending on the type of tear. Recovery involves cast immobilization for four to six weeks after surgery followed by aggressive physical therapy to regain motion and strength.
ANKLE FRACTURE

There are three main bones that make up the ankle joint; the tibia, or shin bone, the fibula, the small bone of the lower leg, and the talus which sits between the ankle joint and the heel. Fractures to the ankle can involve one, or all three bones.
Ankle fractures have a variety of classifications, and treatment depends on location of the fracture, displacement of the bone, number of bones involved, and joint involvement. Ankle fractures most often result from some sort of trauma, and symptoms include pain, swelling, bruising, and possible deformity. Diagnosis is confirmed by X-ray and CT scans, if needed.
If the fracture is not significantly displaced and does not involve more than one bone, a cast can be placed for 4-6 weeks to provide stabilization while the fracture heals. Displaced fractures, fractures with multiple bone fragments, fractures of more than one bone, or fractures with joint involvement or dislocation likely will require surgery using plates and screws to hold the fracture in alignment and allow for healing. After removal of the cast physical therapy is initiated to regain motion and strength.
PLANTAR FASCIITIS
Plantar fasciitis is a very common problem. Plantar fasciitis causes pain at the bottom of the heel and occurs when the strong, and thick, band of tissue that supports the arch of the foot (the plantar fascia) becomes irritated and inflamed.
Plantar fasciitis typically develops over time and without a specific injury or event. Factors that make a patient more prone to developing plantar fasciitis are calf and Achilles tightness, patients with a very high arch, repetitive impact activity such as running and jumping, or bone spurs of the heel at the attachment of the plantar fascia.
Symptoms for this condition include pain on the bottom of the foot near the heel that is worse with the first few steps after getting out of bed in the morning, or after a long period of rest, pain in this area that subsides after a few minutes of walking, and worsening pain after exercise or activity. Diagnosis is made via physical exam and X-rays are helpful to rule out a heel bone.
Majority of patients with plantar fasciitis get better with conservative care. The mainstay of treatment for this issue is stretching and reducing inflammation. Ice, anti-inflammatories, physical therapy, shoe orthotics or heel cups, nighttime splints, and cortisone injections are all options for treatment, and most people do well with these. However, there are surgical options available for refractory cases.
ANKLE CARTILAGE DAMAGE/LOOSE FRAGMENTS
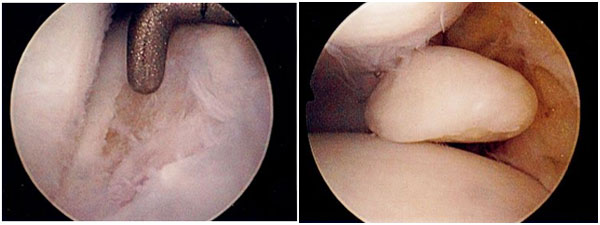
Covering our ankle joint is cartilage. Damage to this cartilage can happen in a number of ways although the most common is arthritis. Arthritis is the breakdown and thinning of cartilage which can lead to large areas of cartilage defect inside the ankle. Localized areas of cartilage damage in an otherwise non-arthritic ankle usually are the result of some sort of trauma causing injury to the cartilage in that area.
Diffuse cartilage damage, like that of arthritis, causes generalized stiffness, soreness and pain. Occasionally, cartilage damage can cause mechanical symptoms inside the ankle such as popping and catching. This is usually from large cartilage flaps or loose fragments inside the ankle that catch during range of motion. X-ray and MRI are used to confirm this.
While no great surgical treatment is available for arthritis, arthroscopy can be done for patients with mechanically symptomatic cartilage damage or loose fragments. The goal behind this minimally invasive procedure is to smooth out the cartilage defects and remove all detached fragments. Cartilage cannot be replaced and arthritis symptoms are still likely to be present even after the surgery. However, popping, catching and clicking associated with the loose fragments and/or cartilage flaps will improve.
Head to our “Treatments” section to read more about this surgery and the recovery process.


